DALLAS — Older adults who live in seniors housing communities live longer, receive more home health services and benefit from greater rehabilitative and preventive care in the two years following move-in than those who do not, according to new research conducted by NORC at the University of Chicago.
The National Investment Center for Seniors Housing & Care (NIC), which commissioned the study, unveiled the findings Tuesday during a press briefing at the Omni Dallas Hotel, site of the 2024 NIC Spring Conference. The three-day event has attracted approximately 1,825 industry professionals.
NORC researchers compared older adults who moved into seniors housing communities in 2017 and resided there for two years or until their death to a similar group of older adults who remained living in the greater community. They analyzed six measures: mortality, days alive, days away from home due to adverse health events, days receiving home health care, preventative and rehabilitative health services days, and days on anti-psychotics to understand the impact of seniors housing.
On average, older adults who move into seniors housing:
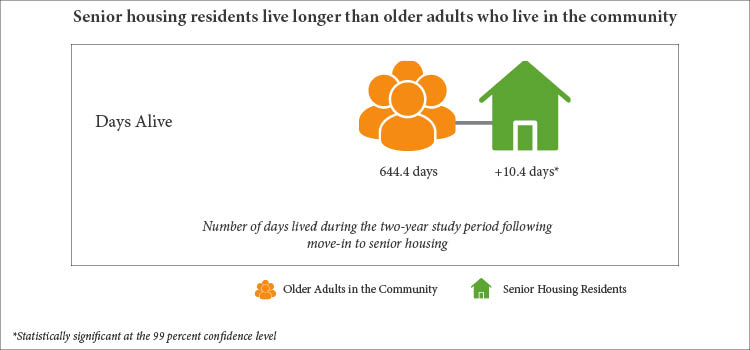
- Live longer — living more than one week longer than older adults who live in the community and have a lower mortality rate;
- Receive more home health care — receiving 10 more days of home health care services than older adults who live in the community;
- Obtain more preventive/rehab services at home — receiving four more days of preventive and rehabilitative services at home than older adults who live in the community;
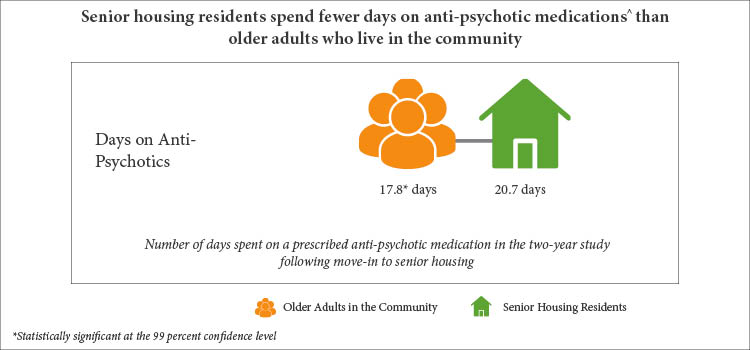
- Spend less time on anti-psychotics — spending three fewer days on anti-psychotics than older adults who live in the community.
The NORC study found that adults who moved into seniors housing properties spend roughly the same number of days away from home to receive high-acuity care as older adults who live in the community at large. As consumers continue to demand more accountability and better outcomes, NIC officials believe there are tremendous opportunities for the senior sector to integrate healthcare and housing to better meet consumer preferences and reduce the cost of care over time.

Researchers also looked at variation across different types of private-pay seniors housing communities, including continuing care retirement communities (CCRCs), independent living communities, assisted living communities, and memory care communities.
- Notably, residents in the top 25 percent of communities live 70 days longer than those in the bottom 25 percent of communities.
- CCRC residents live almost two weeks longer than older adults in the community.
- Seniors housing residents in the top 25 percent of communities receive greater than 40 more days of home health care than their peers in the bottom 25 percent of communities.
The researchers point out that the study was limited to seniors housing properties included in the NIC MAP Vision database. The study was also limited to properties that had 11 or more new residents in 2017 and who continued to live in that community for the duration of the study period (730 days) or until their death. The survey period of 2017-2019 was chosen to ensure the results wouldn’t be tainted by COVID in any way, according to NORC. The COVID pandemic struck the U.S. in the first quarter of 2020.
Observations, insights
“As the proportion of America’s older adults increases, there is growing demand for comprehensive health and wellness support within seniors housing,” said Dianne Munevar, vice president of health care strategy at NORC, in prepared remarks. “Seniors housing operators can capitalize on the growing demand and strengthen the appeal of seniors housing communities by differentiating the scope of preventative health services available in their community relative to what’s available to community-dwelling older adults.”
Munevar was present for Tuesday’s press briefing to recap the study’s findings. She believes the research not only provides a springboard for further dialogue on the ways operators can improve the longevity of their residents, but also highlights what the industry is doing well. “These points can and should be used to promote seniors housing and attract America’s older adults to the high-quality product they provide.”
Ray Braun, president and CEO of NIC, said during Tuesday’s press briefing that the next step for the organization is to figure out how to most effectively get the word out to the business community and consumers about the study’s compelling findings. “We had an operator advisory board meeting this morning. They were very excited to hear this news, and the room was abuzz with ‘How can we get this out to the consumer marketplace?’”
For the past 30 years, operators have anecdotally expressed that a senior’s well-being is enhanced by a move to congregate care setting, said Bob Kramer, co-founder and former chairman of NIC and now a consultant to the organization. This large-scale study on six key metrics provides independent corroboration that seniors housing provides better outcomes for residents compared with their non-congregate care peers living in the community at large, emphasized Kramer during the briefing.
The importance of this comparative analysis can’t be overstated, said Kramer. “NIC’s role is to provide that kind of database insight into what’s happening in our sector.”
When asked if there were any results that surprised her, Munevar pointed to the research team’s findings on the use of anti-psychotic medications. At least 25 percent of properties in some segments of seniors housing don’t use anti-psychotic medications at all, a finding she described as “very positive.”
The study is the third part of a four-part project supported by NIC to assess the health and well-being of seniors housing and care residents. Previous studies provided insights on the vulnerability of seniors housing residents and access to health care providers. The final study will assess health outcomes of residents in senior living settings.
To access the summary report of longevity among seniors housing residents, click here.
— Matt Valley